Cardiovascular diseases have been identified as "public health enemy no. 1" by the World Health Organization.
Cardiovascular diseases kill more people than any other single disease.
The search for reliable preventive methods should be pursued.
Prevention of plaques or stabilization of vulnerable plaques
requires a better understanding of molecular signalling.
Weekly overview on new findings and reviews.
Are mast cells in plaques associated with neovascularization and future cardiovascular events?
Mast cells occur in many tissues and are particularly abundant near the boundaries separating the outer from the internal milieu of the body. Mast cells are key players in inflammatory processes and when activated release their granules into the interstitium. It might, therefore, not be unexpected that mast cells play a role in destabilization of atherosclerotic plaques. Actually, mast cells were found to accumulate in fibrous caps of atherosclerotic plaques and their degranulation was associated with activation of matrix metalloproteinases which are known to destabilize plaques. In the study of Willems et al., it was examined whether links exist between the number of mast cells and the neovascularization in human atherosclerotic plaques. In 270 patients suffering from carotid artery stenosis, atherosclerotic plaques were stained for the presence of mast cells. During a follow-up of 3 years, cardiovascular-related endpoints were assessed. Plaques with high numbers of mast cells exhibited an unstable lipid-rich inflammatory phenotype. It was a particularly important finding that the number of mast cells was positively correlated with microvessel density. Furthermore, patients with high intraplaque numbers of mast cells exhibited more cardiovascular events during the follow-up. Willems et al. concluded that intraplaque mast cell numbers associate with future cardiovascular events. One of the challenges is to find interventions that stabilize mast cells without interfering with their physiological role. Could omega-3 highly unsaturated fatty acids (HUFA) be useful in this context?
Eur Heart J. 2013 Dec;34(48):3699-706. doi: 10.1093/eurheartj/eht186. Epub 2013 Jun 11.
Mast cells in human carotid atherosclerotic plaques are associated with intraplaque microvessel density and the occurrence of future cardiovascular
events.
Willems S, Vink A, Bot I, Quax PH, de Borst GJ, de Vries JP, van de Weg SM, Moll FL, Kuiper J, Kovanen PT, de Kleijn DP, Hoefer IE, Pasterkamp G.
Experimental Cardiology Laboratory (room G02.523), University Medical Centre Utrecht, Heidelberglaan 100, 3584 CX, Utrecht, the Netherlands.
AIMS: Human autopsy, animal, and cell culture studies together have merged in a concept suggesting participation of mast cells (MCs) in the generation of
atherosclerotic plaques. More specifically, these studies have suggested MC-induced intraplaque neovascularization as one mechanism by which MCs may
render the plaques vulnerable. The present study was designed to assess the association between MC numbers and neovascularization in human atherosclerotic
plaques, and to relate the abundance of plaque MCs to the occurrence of adverse cardiovascular events during the follow-up.
METHODS AND RESULTS: Atherosclerotic plaques of 270 patients suffering from carotid artery stenosis were stained for the presence of MCs (MC tryptase).
Furthermore, during a follow-up of 3 years, cardiovascular-related endpoints were assessed in 253 patients. On average a high number of MCs were observed per
plaque cross-section [median 108 (55-233) cells per section]. Plaques with high MC numbers revealed an unstable lipid-rich inflammatory phenotype and were
associated with symptomatic patients. In addition, MC numbers were positively associated with microvessel density (r = 0.416, P < 0.001). Patients with high
intraplaque MC numbers showed significantly more cardiovascular events during the follow-up (58/142 vs. 31/111 events, P = 0.029). In a multivariate analysis with
correction for the main risk factors of cardiovascular diseases, MCs remained independently associated with adverse cardiovascular events (P = 0.025).
CONCLUSION: Mast cells are highly prevalent in human carotid atherosclerotic lesions and associated with plaque microvessel density. Furthermore, intraplaque
MC numbers associate with future cardiovascular events.
Why is
resolution of inflammation impaired in the
atherosclerotic plaque?
Resolution of inflammation involves emigration of monocyte-derived cells out of an inflamed tissue. It has been proposed that this emigration through nearby lymphatic vessels is impaired in atherosclerosis. It has been hypothesized that restoration of the capacity of monocyte-derived cells to leave plaques could facilitate regression of atherosclerosis. Of particular interest is in this context a group of proteins called netrins (from the Sanskrit word “netr”, i.e. “one who guides"). It has been inferred that expression of netrin-1 (NTN1) in plaques would prevent inflammatory cell egress and induce smooth muscle cells recruitment into the intima, thereby promoting lesion progression. It is, therefore, important that Oksala et al. found a dysregulation of the expression of NTN1 in smooth muscle cells and its chemorepulsive receptor UNC5B in macrophages which are involved in the development of atherosclerosis and unstable plaques. NTN1 expression correlated positively with smooth muscle cell proliferation. NTN1 was downregulated and UNC5B upregulated in atherosclerotic plaques. However, no differences were observed when the expression of NTN1 and its receptors was examined in whole blood or circulating monocytes.
Circ Cardiovasc Genet. 2013 Oct 11. [Epub ahead of print]
Association of Neuroimmune Guidance Cue Netrin-1 and its Chemorepulsive Receptor UNC5B with Atherosclerotic Plaque Expression Signatures and Stability in Human(s) - Tampere Vascular Study.
Oksala N, Pärssinen J, Seppälä I, Raitoharju E, Kholová I, Hernesniemi J, Lyytikäinen LP, Levula M, Mäkelä KM, Sioris T, Kähönen M, Laaksonen R, Hytönen V,
Lehtimäki T.
1Department of Clinical Chemistry, Fimlab Laboratories and University of Tampere, School of Medicine & Division of Vascular Surgery, Department of Surgery, Tampere
University Hospital, Tampere, Finland.
BACKGROUND: -Macrophage (MΦ) infiltration and smooth muscle cell (SMC) proliferation are hallmarks of atherosclerosis and unstable plaques. Neuroimmune
guidance cue 1 (netrin-1, NTN1) plays a critical role controlling MΦ trafficking and SMC activation. Characterization of expression of netrin-1 and its receptors
and their association with plaque stability in human(s) is lacking.
METHODS AND RESULTS: -The expression of NTN1 and its receptors did not differ in either whole blood or circulating monocytes from patients with coronary artery
disease (n=55) compared with healthy controls (n=45). However, NTN1 was downregulated (-2.9-fold, p<0.0001) and UNC5B upregulated (2.2-fold, p<0.0001) in
atherosclerotic plaques (n=68) while there were no differences in other NTN1 receptors compared with histologically normal controls (n=28). Increased UNC5B
expression associated with histologically more stable plaques (p=0.011). NTN1 expression correlated positively with SMC markers and signatures and negatively
with inflammatory markers and M1 and especially M2 signatures in the atherosclerotic plaques. UNC5B clustering correlated positively with inflammatory
and MΦ markers. NTN1 protein co-localized with CD68-positive cells of monocytic origin and HHF3-positive cells indicative of SMCs in the plaques and only with
SMCs in the control samples. NTN1 protein was highly expressed in the intimal layer of the control vessels.
CONCLUSIONS: -Present findings provide support for the hypothesis that dysregulation of expression of NTN1 in SMCs and its chemorepulsive receptor UNC5B
in macrophages are involved in the development of atherosclerosis and unstable plaques.
Plaque stabilization by broad-spectrum chemokine inhibition?
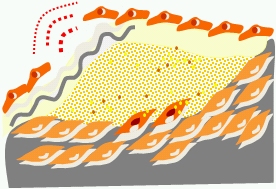
A vulnerable plaque is characterized by a thin fibrous cap and accumulation of various pro-inflammatory factors. There is increasing evidence that plaque macrophages are not only innocent bystanders but are causally involved in plaque destabilization. This might be surprising since the function of tissue macrophages is to remove dead cell debris and to attack microorganisms. In addition to this phagocytosis and antigen presentation they produce various cytokines which can have a pro-inflammatory action. In addition, they produce matrix degrading enzymes which can contribute to thinning of the plaque cap (as schematically shown in the animated logo of our Plaque News). To what extent and how specific should one interfere with cytokine production? Of recent interest is in this respect a treatment with broad-spectrum chemokine inhibitors. It was shown by Reckless et al. that treatment of apolipoprotein-E-deficient mice with the chemokine inhibitor NR58-3.14.3 had 30-40% fewer macrophages in vascular lesions. Furthermore, total collagen I staining and smooth muscle cell number were increased, suggesting that a shift to a more stable plaque phenotype had been achieved. It was concluded by Reckless et al. that attenuation of macrophage accumulation by chemokine inhibition may be useful for promoting plaque stabilization. This pioneering study leads to the question whether other "broad-band" chemokine inhibitors are available. In particular, whether the omega-3 fatty acid EPA (20:5n-3) which antagonizes arachidonic acid (20:4n-6) and some of its subsequent pro-inflammatory cytokines has a similar action. Our work is in progress ...
J Vasc Res. 2005 Nov-Dec;42(6):492-502. Epub 2005 Sep 7.
Broad-spectrum chemokine inhibition reduces vascular macrophage accumulation and collagenolysis consistent with plaque stabilization in mice.
Reckless J, Tatalick L, Wilbert S, McKilligin E, Grainger DJ.
Department of Medicine, University of Cambridge, Addenbrooke's Hospital, Cambridge, UK. jr219@cam.ac.uk
Plaque destabilization: how do dendritic cells and T cells interact?
Dendritic cells are present in tissues which are in contact with the external environment. When activated, dendritic cells interact with T and B cells to initiate the immune response. They process antigen material and present it on the surface to other cells. Dendritic cells can, however, also be involved in immunological disorders and have been found in atherosclerotic plaques where they appear to contribute to plaque destabilization through activation of T cells. Dietel et al. provide novel insights into the interaction of dendritic cells and regulatory T cells in plaque inflammation and stability: When compared with stable plaques, the number of dendritic cells was increased in the inflammatory plaque shoulder of vulnerable plaques, while regulatory T cells were reduced. This inverse correlation and the association of the observed infiltration rates with plaque stability, were confirmed by PCR.
Atherosclerosis. 2013;230:92-9. doi:10.1016/j.atherosclerosis.2013.06.014. Epub 2013 Jul 10.
Decreased numbers of regulatory T cells are associated with human atherosclerotic lesion vulnerability and inversely correlate with infiltrated mature dendritic
cells.
Dietel B, Cicha I, Voskens CJ, Verhoeven E, Achenbach S, Garlichs CD.
Department of Cardiology and Angiology, University Hospital Erlangen, Erlangen, Germany. Electronic address: barbara.dietel@uk-erlangen.de.
Links between vascular calcification - inflammation - plaque instability: a role of galectin-3 and receptor for advanced lipoxidation/glycation endproducts (ALEs/AGEs)?
"Carbonyl stress" appears to be of great importance also in atherosclerosis. Carbonyl stress can alter the structure and function of cellular and matrix proteins. It involves irreversible nonenzymatic protein modifications by carbohydrates or lipids, i.e., AGE/ALE. Of particular interest, proteins can be modified by various oxidation products of polyunsaturated fatty acids (arachidonic acid, EPA and DHA). Examples of peroxidation products are glyoxal, malondialdehyde, hydroxynonenal, and acrolein (Miyata et al.: Advanced Glycation and Lipoxidation End Products: Role of Reactive Carbonyl Compounds Generated during Carbohydrate and Lipid Metabolism). It should be noted that dietar fish oils can also be a source of various oxidation products such as aldehydes (Rupp et al. Replacement of Reduced Highly Unsaturated
Fatty Acids (HUFA Deficiency) in Dilative Heart Failure: Dosage of EPA/DHA and Variability of Adverse Peroxides and Aldehydes in Dietary Supplement Fish Oils). There remains, however, the need of understanding the signalling of ALEs derived from oxidation products. Menini et al. studied the roles of galectin-3 and receptor for AGEs (RAGE), two ALEs/AGEs-receptors with diverging effects on inflammation and bone metabolism, in the process of vascular calcification. They derive a novel molecular mechanism by which galectin-3 and RAGE modulate in divergent ways, not only inflammation, but also vascular osteogenesis, by modulating Wnt/β-catenin signalling and independently of ALEs/AGEs.
Cardiovasc Res. 2013 Aug 23. [Epub ahead of print]
The galectin-3/RAGE dyad modulates vascular osteogenesis in atherosclerosis.
Menini S, Iacobini C, Ricci C, Fantauzzi CB, Salvi L, Pesce CM, Relucenti M, Familiari G, Taurino M, Pugliese G.
From the Department of Clinical and Molecular Medicine.
Vulnerable vs. stable plaques: are genes differentially expressed?
In simple terms, we know why plaques become unstable or vulnerable. We are also aware of the high risk of myocardial infarction or stroke that is associated with vulnerable plaques. How can the transition from stable to unstable plaque be prevented? Clearly we need to improve our knowledge on the molecular signalling involved in the destabilization of plaques. Salem et al. provide the important information that between stable and unstable plaques of TIA/stroke patients 346 genes are differentially expressed (293 down-regulated and 53 up-regulated). The findings confirm the intuitively held belief that changes in chemokine and protein signalling (pro-inflammatory/pro-apoptotic) may be associated with acute plaque disruption and precede the onset of symptoms. It was concluded that these genes could become targets for innovative medical treatments in the future or could help identify asymptomatic patients with unstable plaques.
Eur J Vasc Endovasc Surg. 2013 Feb;45(2):121-7. doi: 10.1016/j.ejvs.2012.11.006.
Histologically unstable asymptomatic carotid plaques have altered expression of genes involved in chemokine signalling leading to localised plaque inflammation
and rupture.
Salem MK, Vijaynagar B, Sayers RD, West K, Moore D, Robinson TG, Naylor AR, Bown MJ.
Vascular Surgery Group, Department of Cardiovascular Sciences, University of Leicester, LE2 7LX, UK. ms447@le.ac.uk
28.12.2013 (HR)
Resolution of inflammation involves emigration of monocyte-derived cells out of an inflamed tissue. It has been proposed that this emigration through nearby lymphatic vessels is impaired in atherosclerosis. It has been hypothesized that restoration of the capacity of monocyte-derived cells to leave plaques could facilitate regression of atherosclerosis. Of particular interest is in this context a group of proteins called netrins (from the Sanskrit word “netr”, i.e. “one who guides"). It has been inferred that expression of netrin-1 (NTN1) in plaques would prevent inflammatory cell egress and induce smooth muscle cells recruitment into the intima, thereby promoting lesion progression. It is, therefore, important that Oksala et al. found a dysregulation of the expression of NTN1 in smooth muscle cells and its chemorepulsive receptor UNC5B in macrophages which are involved in the development of atherosclerosis and unstable plaques. NTN1 expression correlated positively with smooth muscle cell proliferation. NTN1 was downregulated and UNC5B upregulated in atherosclerotic plaques. However, no differences were observed when the expression of NTN1 and its receptors was examined in whole blood or circulating monocytes.
Circ Cardiovasc Genet. 2013 Oct 11. [Epub ahead of print]
Association of Neuroimmune Guidance Cue Netrin-1 and its Chemorepulsive Receptor UNC5B with Atherosclerotic Plaque Expression Signatures and Stability in Human(s) - Tampere Vascular Study.
Oksala N, Pärssinen J, Seppälä I, Raitoharju E, Kholová I, Hernesniemi J, Lyytikäinen LP, Levula M, Mäkelä KM, Sioris T, Kähönen M, Laaksonen R, Hytönen V,
Lehtimäki T.
1Department of Clinical Chemistry, Fimlab Laboratories and University of Tampere, School of Medicine & Division of Vascular Surgery, Department of Surgery, Tampere
University Hospital, Tampere, Finland.
BACKGROUND: -Macrophage (MΦ) infiltration and smooth muscle cell (SMC) proliferation are hallmarks of atherosclerosis and unstable plaques. Neuroimmune
guidance cue 1 (netrin-1, NTN1) plays a critical role controlling MΦ trafficking and SMC activation. Characterization of expression of netrin-1 and its receptors
and their association with plaque stability in human(s) is lacking.
METHODS AND RESULTS: -The expression of NTN1 and its receptors did not differ in either whole blood or circulating monocytes from patients with coronary artery
disease (n=55) compared with healthy controls (n=45). However, NTN1 was downregulated (-2.9-fold, p<0.0001) and UNC5B upregulated (2.2-fold, p<0.0001) in
atherosclerotic plaques (n=68) while there were no differences in other NTN1 receptors compared with histologically normal controls (n=28). Increased UNC5B
expression associated with histologically more stable plaques (p=0.011). NTN1 expression correlated positively with SMC markers and signatures and negatively
with inflammatory markers and M1 and especially M2 signatures in the atherosclerotic plaques. UNC5B clustering correlated positively with inflammatory
and MΦ markers. NTN1 protein co-localized with CD68-positive cells of monocytic origin and HHF3-positive cells indicative of SMCs in the plaques and only with
SMCs in the control samples. NTN1 protein was highly expressed in the intimal layer of the control vessels.
CONCLUSIONS: -Present findings provide support for the hypothesis that dysregulation of expression of NTN1 in SMCs and its chemorepulsive receptor UNC5B
in macrophages are involved in the development of atherosclerosis and unstable plaques.
Plaque stabilization by broad-spectrum chemokine inhibition?
A vulnerable plaque is characterized by a thin fibrous cap and accumulation of various pro-inflammatory factors. There is increasing evidence that plaque macrophages are not only innocent bystanders but are causally involved in plaque destabilization. This might be surprising since the function of tissue macrophages is to remove dead cell debris and to attack microorganisms. In addition to this phagocytosis and antigen presentation they produce various cytokines which can have a pro-inflammatory action. In addition, they produce matrix degrading enzymes which can contribute to thinning of the plaque cap (as schematically shown in the animated logo of our Plaque News). To what extent and how specific should one interfere with cytokine production? Of recent interest is in this respect a treatment with broad-spectrum chemokine inhibitors. It was shown by Reckless et al. that treatment of apolipoprotein-E-deficient mice with the chemokine inhibitor NR58-3.14.3 had 30-40% fewer macrophages in vascular lesions. Furthermore, total collagen I staining and smooth muscle cell number were increased, suggesting that a shift to a more stable plaque phenotype had been achieved. It was concluded by Reckless et al. that attenuation of macrophage accumulation by chemokine inhibition may be useful for promoting plaque stabilization. This pioneering study leads to the question whether other "broad-band" chemokine inhibitors are available. In particular, whether the omega-3 fatty acid EPA (20:5n-3) which antagonizes arachidonic acid (20:4n-6) and some of its subsequent pro-inflammatory cytokines has a similar action. Our work is in progress ...
J Vasc Res. 2005 Nov-Dec;42(6):492-502. Epub 2005 Sep 7.
Broad-spectrum chemokine inhibition reduces vascular macrophage accumulation and collagenolysis consistent with plaque stabilization in mice.
Reckless J, Tatalick L, Wilbert S, McKilligin E, Grainger DJ.
Department of Medicine, University of Cambridge, Addenbrooke's Hospital, Cambridge, UK. jr219@cam.ac.uk
Plaque destabilization: how do dendritic cells and T cells interact?
Dendritic cells are present in tissues which are in contact with the external environment. When activated, dendritic cells interact with T and B cells to initiate the immune response. They process antigen material and present it on the surface to other cells. Dendritic cells can, however, also be involved in immunological disorders and have been found in atherosclerotic plaques where they appear to contribute to plaque destabilization through activation of T cells. Dietel et al. provide novel insights into the interaction of dendritic cells and regulatory T cells in plaque inflammation and stability: When compared with stable plaques, the number of dendritic cells was increased in the inflammatory plaque shoulder of vulnerable plaques, while regulatory T cells were reduced. This inverse correlation and the association of the observed infiltration rates with plaque stability, were confirmed by PCR.
Atherosclerosis. 2013;230:92-9. doi:10.1016/j.atherosclerosis.2013.06.014. Epub 2013 Jul 10.
Decreased numbers of regulatory T cells are associated with human atherosclerotic lesion vulnerability and inversely correlate with infiltrated mature dendritic
cells.
Dietel B, Cicha I, Voskens CJ, Verhoeven E, Achenbach S, Garlichs CD.
Department of Cardiology and Angiology, University Hospital Erlangen, Erlangen, Germany. Electronic address: barbara.dietel@uk-erlangen.de.
Links between vascular calcification - inflammation - plaque instability: a role of galectin-3 and receptor for advanced lipoxidation/glycation endproducts (ALEs/AGEs)?
"Carbonyl stress" appears to be of great importance also in atherosclerosis. Carbonyl stress can alter the structure and function of cellular and matrix proteins. It involves irreversible nonenzymatic protein modifications by carbohydrates or lipids, i.e., AGE/ALE. Of particular interest, proteins can be modified by various oxidation products of polyunsaturated fatty acids (arachidonic acid, EPA and DHA). Examples of peroxidation products are glyoxal, malondialdehyde, hydroxynonenal, and acrolein (Miyata et al.: Advanced Glycation and Lipoxidation End Products: Role of Reactive Carbonyl Compounds Generated during Carbohydrate and Lipid Metabolism). It should be noted that dietar fish oils can also be a source of various oxidation products such as aldehydes (Rupp et al. Replacement of Reduced Highly Unsaturated
Fatty Acids (HUFA Deficiency) in Dilative Heart Failure: Dosage of EPA/DHA and Variability of Adverse Peroxides and Aldehydes in Dietary Supplement Fish Oils). There remains, however, the need of understanding the signalling of ALEs derived from oxidation products. Menini et al. studied the roles of galectin-3 and receptor for AGEs (RAGE), two ALEs/AGEs-receptors with diverging effects on inflammation and bone metabolism, in the process of vascular calcification. They derive a novel molecular mechanism by which galectin-3 and RAGE modulate in divergent ways, not only inflammation, but also vascular osteogenesis, by modulating Wnt/β-catenin signalling and independently of ALEs/AGEs.
Cardiovasc Res. 2013 Aug 23. [Epub ahead of print]
The galectin-3/RAGE dyad modulates vascular osteogenesis in atherosclerosis.
Menini S, Iacobini C, Ricci C, Fantauzzi CB, Salvi L, Pesce CM, Relucenti M, Familiari G, Taurino M, Pugliese G.
From the Department of Clinical and Molecular Medicine.
Vulnerable vs. stable plaques: are genes differentially expressed?
In simple terms, we know why plaques become unstable or vulnerable. We are also aware of the high risk of myocardial infarction or stroke that is associated with vulnerable plaques. How can the transition from stable to unstable plaque be prevented? Clearly we need to improve our knowledge on the molecular signalling involved in the destabilization of plaques. Salem et al. provide the important information that between stable and unstable plaques of TIA/stroke patients 346 genes are differentially expressed (293 down-regulated and 53 up-regulated). The findings confirm the intuitively held belief that changes in chemokine and protein signalling (pro-inflammatory/pro-apoptotic) may be associated with acute plaque disruption and precede the onset of symptoms. It was concluded that these genes could become targets for innovative medical treatments in the future or could help identify asymptomatic patients with unstable plaques.
Eur J Vasc Endovasc Surg. 2013 Feb;45(2):121-7. doi: 10.1016/j.ejvs.2012.11.006.
Histologically unstable asymptomatic carotid plaques have altered expression of genes involved in chemokine signalling leading to localised plaque inflammation
and rupture.
Salem MK, Vijaynagar B, Sayers RD, West K, Moore D, Robinson TG, Naylor AR, Bown MJ.
Vascular Surgery Group, Department of Cardiovascular Sciences, University of Leicester, LE2 7LX, UK. ms447@le.ac.uk
28.12.2013 (HR)