this statement by the late R.E.
Beamish (Can J Cardiol 1994;10:603) summarizes the current
therapy for heart failure. All known drugs prolong survival but
cannot prevent final failure of the heart. Therefore,
cardiovascular diseases have been identified as "public health
enemy No. 1" by the World Health Organization. Cardiovascular
diseases kill more people than any other single disease. The
search for reliable preventive methods should vigorously be
pursued.
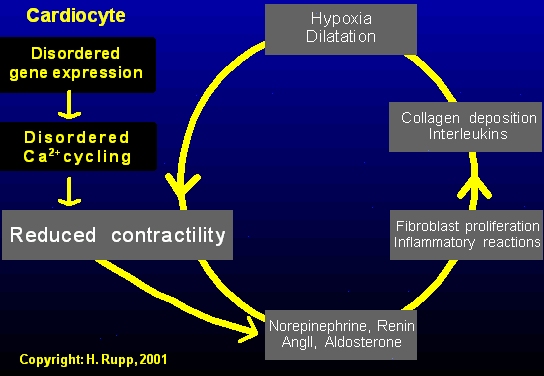
The image shows various drug
targets during the progression of congestive heart failure
(CHF). Surprisingly, various potential targets have not been
explored, simply because they do not provide an acute
improvement of heart function but rather alter gene expression
of the cardiomyocyte.
An athlete's big heart does not fail!
| PATHOLOGICAL
OVERLOAD & HYPERTROPHY A high blood pressure and coronary artery disease are the major risk factors for heart failure. Heart failure is typically associated with ventricular hypertrophy. The increase in cardiac mass can be considered as an attempt to compensate for the the reduced performance of heart muscle. It is our working hypothesis that hypertrophy should not necessarily be associated with an increased risk of cardiac failure. |
ATHLETE'S
HEART: NORMAL HYPERTROPHY Because an athlete's heart does not fail, specific defects have to exist in hearts with a pathological overload. Novel drug interventions focussing at overloaded hearts should ideally restore a normal pump function by normalizing molecular structures of the cardiomyocyte. It is our working hypothesis that these 'transcriptional modulators' prevent progression of heart failure. |
Because the pump function of the heart is derived from the contraction of individual cardiomyocytes, the overall function of heart muscle is reduced. This depressed function is counteracted by the body using mechanisms that are appropriate for acute adjustment of heart performance, e.g. due to postural changes or blood loss.
A vicious cycle is initiated involving neuro-endocrine activation involving the sympathetic nervous system and the renin-angiotensin II-aldosterone system (RAAS). Although the neuro-endocrine activation results in an apparently improved pump function of the heart, a remodeling of the extracellular matrix occurs further aggrevating the impaired pump function of the heart.
As a consequence of the enhanced
catecholamine, angiotensin II and aldosterone influences,
collagen synthesis is stimulated resulting in an enhanced
collagen deposition, i.e. fibrosis of the heart. The increased
collagen content of the heart has various detrimental actions on
the mechanical performance, e.g. increased stiffness, and
provides therefore a further stimulus for neuroendocrine
activation.
Any depression of cardiomyocyte function should be prevented. Currently available drugs appear not to be designed for this target. We have identified agents which selectively improve the function of overloaded hearts by interfering with the gene expression of cardiomyocytes, i.e. 'transcriptional modulators'. We hypothesize that early interference with defects in gene expression of cardiomyocytes prevents the deletrious neuro-endocrine activation.
If neuro-endocrine activation has
already occurred because the progression has not been diagnosed,
drugs are needed targeted at the sympathetic overactivity and
activation of the renin-angiotensin II-aldosterone system. These
drugs prolong life expectancy but cannot prevent congestive
heart failure. A combination with selective 'transcriptional
modulators' targeted at gene expression of cardiomyocytes is
hypothesized to contribute to prevention of heart failure.


For information on drug-induced
modulation of gene expression of the cardiomyocyte, please
contact Heinz
Rupp, Ph.D., Professor of Physiology,
personal data, Google
Scholar
Citations
Publications on
cardiovascular effects of etomoxir
Patents for use
of etomoxir in treatment of heart failure
For information on drug-induced modulation of extracellular matrix remodeling, please contact Christian G. Brilla, M.D., Ph.D., Professor of Medicine, personal data.
last modified August 23, 2013 by Heinz Rupp